Examining the Link Between Glucagon-Like Peptide-1 Receptor Agonists and Neovascular Age-Related Macular Degeneration Risk
Examining the Link Between Glucagon-Like Peptide-1 Receptor Agonists and Neovascular Age-Related Macular Degeneration Risk

A recent cohort study published in JAMA Ophthalmology has unveiled a potentially alarming association between the use of glucagon-like peptide-1 receptor agonists (GLP-1 RAs) and the development of neovascular age-related macular degeneration (AMD) in patients with diabetes. GLP-1 RAs, widely regarded for their efficacy in managing blood glucose levels and providing cardiovascular benefits, have now been linked to a twofold increase in the risk of incident neovascular AMD compared to diabetic patients who do not receive these agents. This unexpected finding calls for a re-evaluation of the safety profile of GLP-1 RAs in the context of ocular health.
GLP-1 receptor agonists operate by mimicking the incretin hormone GLP-1, which enhances insulin secretion, suppresses glucagon release, and slows gastric emptying. These mechanisms collectively improve glycemic control in type 2 diabetes mellitus. Over recent years, GLP-1 RAs have gained prominence not only for their glucose-lowering properties but also for their demonstrated cardiovascular and renal benefits. However, the implications of GLP-1 receptor activation beyond metabolic regulation have remained largely unexplored until now.
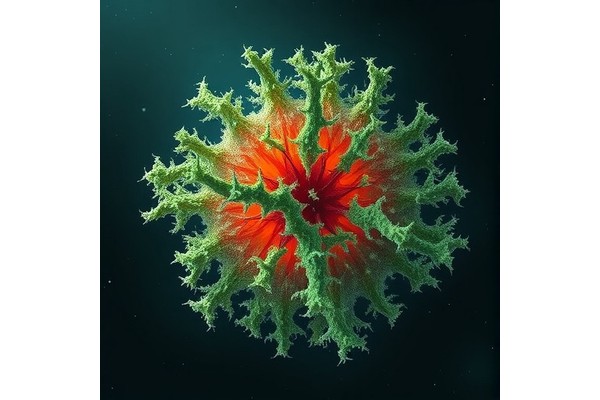
Age-related macular degeneration is a leading cause of irreversible vision loss among elderly populations globally. The neovascular or "wet" form of AMD is characterized by the proliferation of aberrant blood vessels beneath the retina, leading to leakage, hemorrhage, and subsequent photoreceptor damage. Understanding the risk factors that contribute to the pathogenesis of neovascular AMD is critical for preventing vision impairment. The revelation of a potential connection between GLP-1 RAs and AMD introduces a new variable in the complex etiology of this disease.
The study design involved a longitudinal cohort analysis encompassing patients diagnosed with diabetes, comparing those treated with GLP-1 receptor agonists against a matched control group not receiving these therapies. The observation that GLP-1 RA users manifested a doubled risk of developing neovascular AMD prompts significant clinical concern. Importantly, the findings were adjusted for known confounders such as age, baseline glycemic control, and other systemic comorbidities, strengthening the validity of the association.
From a mechanistic standpoint, the biological rationale underlying this correlation remains speculative but intriguing. GLP-1 receptors are expressed in various ocular tissues, suggesting that pharmacologic agonism could influence retinal microvascular physiology. The proangiogenic or inflammatory pathways possibly triggered by GLP-1 RA exposure warrant thorough scientific investigation. It is conceivable that receptor activation may induce local vascular endothelial growth factor (VEGF) expression or modulate immune responses, thereby facilitating choroidal neovascularization.
Clinical implications of these findings are profound yet complex. While GLP-1 receptor agonists offer substantial benefits in glycemic regulation and cardiovascular risk mitigation, their potential to elevate the risk of sight-threatening AMD necessitates a careful assessment of risk versus benefit. Physicians prescribing GLP-1 RAs for diabetic patients with pre-existing ocular vulnerabilities or advanced age might need to exercise increased vigilance, instituting regular ophthalmological evaluations to promptly detect early signs of AMD.
Further research is imperative to elucidate the pathophysiological mechanisms linking GLP-1 receptor agonism to neovascular AMD. Prospective studies incorporating detailed retinal imaging, biomarker analysis, and pharmacodynamic profiling could shed light on this association. Moreover, preclinical models exploring the impact of GLP-1 RAs on retinal angiogenesis and inflammation might provide actionable insights to guide clinical practice.
In the meantime, patients receiving GLP-1 receptor agonists should not discontinue their medication without consulting healthcare providers, as the overall benefits can be significant. Rather, awareness of potential ocular side effects should be raised among clinicians and patients alike. Interdisciplinary collaboration between endocrinologists, ophthalmologists, and pharmacologists will be critical to optimize patient outcomes and formulate monitoring guidelines.
This study also underscores the broader theme that systemic medications may exert off-target effects in discrete tissues such as the retina, influencing disease trajectories in unanticipated ways. As pharmacotherapy evolves with novel agents and mechanisms, post-marketing surveillance and real-world evidence assume greater importance in safeguarding patient safety.
To summarize, the newly reported association between GLP-1 receptor agonist use and a heightened risk of neovascular age-related macular degeneration in diabetic populations introduces a compelling area for further exploration. The complexity of diabetic care mandates balancing multiple organ system risks and benefits, and ocular health must be considered a vital component within this matrix. The cautionary findings raise the prospect of personalized treatment strategies attentive not only to metabolic targets but also to preserving visual function.
As research advances, it will be crucial to integrate these findings with evolving therapeutic landscapes, potentially leading to stratified approaches where genetic or phenotypic markers inform drug selection. Ultimately, this line of inquiry strives to enhance comprehensive care for patients grappling with diabetes and associated complications.
Subject of Research: Glucagon-like peptide-1 receptor agonist use and risk of neovascular age-related macular degeneration in patients with diabetes
Article Title: [Not provided]
News Publication Date: [Not provided]
Web References: [Not provided]
References: doi:10.1001/jamaophthalmol.2025.1455
Keywords: Macular degeneration, Peptides, Agonists, Diabetes, Risk factors, Cohort studies, Ophthalmology, Developmental stages
Youth-Centred Approaches Transform Mental Health Care
Next PostFish ‘Beauty Salons’ Reveal Microbial Movement Patterns Within Coral Reefs
Ancient Insects Thrive in South American Amber Deposit, Revealing a Vibrant Paleoecosystem